Rapid heart rate disorders are a common source of anxiety for patients and confusion for non-specialists. Among these, the comparison of svt vs sinus tach is one of the most frequently discussed topics in cardiology and emergency medicine. Although both conditions present with a fast heartbeat, their causes, clinical significance, diagnosis, and management differ substantially. Understanding these differences is essential for accurate diagnosis, appropriate treatment, and patient reassurance.
This article explores svt vs sinus tach in depth, explaining how each condition develops, how they appear clinically, and why distinguishing between them matters. By the end, readers will have a clear, practical understanding of these two types of tachycardia and how clinicians approach them in real-world settings.
SVT vs Sinus Tach: Overview of Rapid Heart Rhythms
The human heart beats in response to electrical impulses generated by specialized tissue. Under normal circumstances, these impulses originate from the sinoatrial node, commonly referred to as the heart’s natural pacemaker. When the heart rate exceeds 100 beats per minute, the rhythm is classified as tachycardia.
In discussions about svt vs sinus tach, the key distinction lies in the origin and regulation of these electrical impulses. Sinus tachycardia represents a normal physiological response to internal or external stressors, while supraventricular tachycardia, often abbreviated as SVT, is typically caused by an abnormal electrical circuit above the ventricles.
Although both conditions can produce similar symptoms, their underlying mechanisms are very different, which directly influences treatment strategies and long-term outcomes.
Sinus Tachycardia Explained in the Context of SVT vs Sinus Tach
Sinus tachycardia occurs when the sinoatrial node fires impulses faster than normal, but in an otherwise healthy and organized manner. This type of tachycardia is considered a normal response to situations that increase the body’s demand for oxygen or blood flow.
Common triggers include physical exertion, emotional stress, fever, dehydration, pain, anemia, infection, pregnancy, and stimulant use such as caffeine or nicotine. In these cases, the heart rate increases gradually and decreases once the underlying cause is addressed.
From a physiological standpoint, sinus tachycardia is adaptive rather than pathological. It reflects the body’s attempt to maintain adequate circulation. In the comparison of svt vs sinus tach, this adaptive nature is a defining feature of sinus tachycardia.
SVT vs Sinus Tach: Understanding Supraventricular Tachycardia
Supraventricular tachycardia refers to a group of abnormal heart rhythms that originate above the ventricles but outside the sinoatrial node. Unlike sinus tachycardia, SVT is usually caused by an electrical short circuit or reentry pathway within the atria or the atrioventricular node.
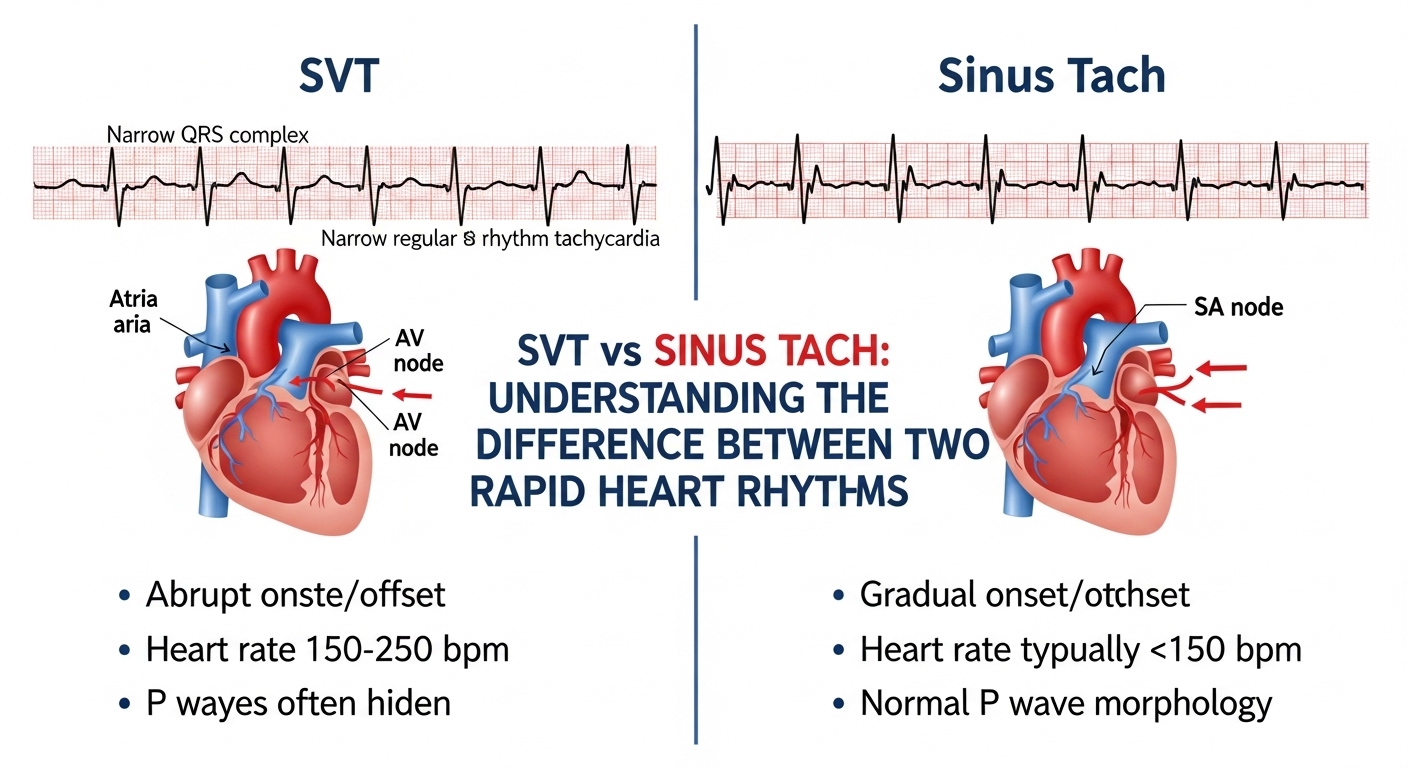
SVT often begins suddenly and ends abruptly, a feature commonly described as paroxysmal onset and termination. Heart rates during SVT are typically higher than those seen in sinus tachycardia and may exceed 150 beats per minute even at rest.
In the framework of svt vs sinus tach, SVT is considered an arrhythmia, meaning it represents an abnormal rhythm rather than a normal physiological response.
SVT vs Sinus Tach: Causes and Mechanisms Compared
Understanding the causes behind each condition is central to differentiating svt vs sinus tach. While both result in rapid heartbeats, the mechanisms driving them are fundamentally different.
Sinus tachycardia is driven by increased sympathetic nervous system activity or reduced parasympathetic tone. This results in faster firing of the sinoatrial node while preserving normal electrical conduction through the heart.
SVT, on the other hand, is caused by abnormal electrical pathways. These pathways may be congenital or acquired and allow electrical impulses to loop repeatedly, producing rapid and sustained heart rates independent of normal physiological demands.
The table below summarizes the core differences in mechanisms:
| Feature | Sinus Tachycardia | Supraventricular Tachycardia |
|---|---|---|
| Electrical origin | Sinoatrial node | Atria or AV node |
| Nature | Physiological response | Pathological arrhythmia |
| Onset | Gradual | Sudden |
| Termination | Gradual | Abrupt |
| Trigger dependency | Yes | Often no |
SVT vs Sinus Tach: Differences in Symptoms and Patient Experience
Symptoms play a major role in how patients perceive even though symptom overlap is common. Both conditions may cause palpitations, lightheadedness, shortness of breath, chest discomfort, and fatigue.
Sinus tachycardia symptoms often correlate with the underlying cause. For example, a patient with fever or dehydration may notice a fast heart rate accompanied by weakness or thirst. Once the trigger resolves, symptoms usually improve.
SVT symptoms tend to be more dramatic and sudden. Patients frequently describe a racing or pounding heartbeat that starts without warning. Anxiety, chest pressure, and near-syncope are more common during SVT episodes, particularly when the heart rate is very high.
In evaluating clinicians pay close attention to how and when symptoms begin, as this often provides crucial diagnostic clues.
SVT vs Sinus Tach: Electrocardiogram Characteristics
The electrocardiogram is one of the most important tools in distinguishing. While both rhythms show rapid rates, their ECG patterns differ in meaningful ways.
In sinus tachycardia, the ECG shows a normal P wave before every QRS complex, with consistent morphology and axis. The rhythm remains regular, and the rate typically fluctuates based on activity or stress levels.
SVT may show absent or abnormal P waves, depending on the specific subtype. In some cases, P waves are hidden within the QRS complex or appear immediately after it. The rhythm is usually very regular, and the rate often remains fixed until the episode terminates.
The table below highlights common ECG distinctions:
| ECG Feature | Sinus Tachycardia | SVT |
|---|---|---|
| P waves | Normal and visible | Absent, hidden, or abnormal |
| Rate variability | Variable | Fixed |
| Rhythm regularity | Regular | Regular |
| Response to activity | Increases and decreases | Often unchanged |
SVT vs Sinus Tach: Diagnostic Approach in Clinical Practice
When evaluating, clinicians rely on a combination of patient history, physical examination, ECG findings, and laboratory testing. The goal is to determine whether the rapid heart rate is a normal physiological response or an abnormal arrhythmia.
Sinus tachycardia is often diagnosed by identifying an underlying cause such as infection, anemia, or anxiety. Blood tests, imaging, and vital signs help confirm these triggers.
SVT diagnosis may require additional monitoring, such as Holter monitors or event recorders, especially if episodes are intermittent. In some cases, electrophysiological studies are performed to identify the exact electrical pathway involved.
Correct diagnosis is essential, as misclassifying can lead to unnecessary treatments or missed opportunities for curative therapy.
SVT vs Sinus Tach: Treatment Strategies and Management
Treatment differences further highlight the importance of distinguishing . Since sinus tachycardia is a response to another condition, management focuses on treating the underlying cause rather than the heart rate itself.
For example, treating dehydration with fluids or managing fever with antipyretics often resolves sinus tachycardia without the need for cardiac medications.
SVT treatment is more rhythm-focused. Acute episodes may be terminated with vagal maneuvers or medications that slow conduction through the atrioventricular node. In recurrent cases, catheter ablation may be offered as a definitive treatment with high success rates.
The following table summarizes management principles:
| Aspect | Sinus Tachycardia | SVT |
|---|---|---|
| Primary treatment | Address underlying cause | Rhythm control |
| Medication role | Limited | Common |
| Curative options | Not applicable | Catheter ablation |
| Long-term prognosis | Excellent | Excellent with treatment |
SVT vs Sinus Tach: Prognosis and Long-Term Outlook
The prognosis for both conditions is generally favorable, but it differs in important ways. In the comparison of sinus tachycardia almost always resolves once the precipitating factor is managed. It rarely leads to long-term cardiac complications in otherwise healthy individuals.
SVT also carries an excellent prognosis, particularly when properly diagnosed and treated. While episodes can be distressing, they are rarely life-threatening in structurally normal hearts. Advances in electrophysiology have made curative treatments widely accessible.
Understanding prognosis helps reduce patient anxiety, which itself can exacerbate symptoms in both conditions.
SVT vs Sinus Tach: Special Considerations in Different Populations
Age, pregnancy, and underlying medical conditions can influence how svt vs sinus tach presents and is managed. In children and adolescents, SVT is one of the most common arrhythmias and may present differently than in adults.
During pregnancy, sinus tachycardia is common due to increased blood volume and metabolic demand. SVT can also occur and requires careful management to balance maternal and fetal safety.
In patients with structural heart disease, distinguishing becomes even more critical, as treatment decisions may carry higher risk.
SVT vs Sinus Tach: Why Accurate Differentiation Matters
Misinterpreting can lead to unnecessary anxiety, inappropriate medication use, or delayed treatment. A patient with sinus tachycardia may be mistakenly treated with antiarrhythmic drugs, while a patient with SVT may be reassured incorrectly and left untreated.
Accurate differentiation ensures that patients receive care tailored to the true nature of their condition. It also empowers patients with knowledge, allowing them to understand their symptoms and participate actively in their treatment decisions.
Conclusion
The comparison of svt vs sinus tach highlights how two conditions with similar outward appearances can differ profoundly in origin, significance, and management. Sinus tachycardia is typically a normal, adaptive response to physiological stress, while SVT represents an abnormal electrical rhythm requiring targeted intervention.
By understanding the mechanisms, symptoms, diagnostic features, and treatments associated with each, clinicians and patients alike can navigate rapid heart rate episodes with confidence and clarity. Knowledge remains the most effective tool in reducing fear, improving outcomes, and ensuring appropriate care in cases of tachycardia.